Practicing in urban southeast Asia a seven-year-old girl presents after several weeks of progressive left leg pain and inability to walk. Over a month ago the girl had a fever. Her father was concerned and went to the local pharmacy. The pharmacy provided the father with an intramuscular injectable anti-pyretic. The father injected the medicine into her upper left leg.
The patient presented with a fever and was ill appearing. She was unable to range her left hip or walk due to pain. There was no apparent cellulitis or subcutaneous abscess. She was admitted for intravenous antibiotics and fluids. The admitting physicians were most concerned about a septic joint, but the diagnosis could also be pyomyositis (a common diagnosis in this region). A radiograph of the left hip and knee were done and interpreted as unremarkable. All other imaging was unavailable. A surgical consultation was ordered, but without imaging the surgeon was not willing to attempt any intervention.
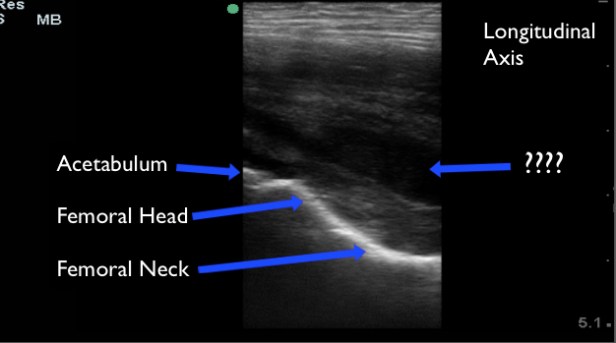
Upon our arrival to the hospital we performed a musculoskeletal POCUS of the bilateral hips. POCUS of the hip joint is best accomplished with the high frequency or linear probe in the pediatric patient, but low frequency probes may be used if the linear probe is unavailable. To evaluate the hip for an effusion with POCUS begin just medial to the ASIS, in a slightly oblique-sagittal plane. This will give you a longitudinal view of the hip joint. Identify the femoral head and acetabulum, followed by the femoral neck inferiorly. Hip effusions typically appear as an anechoic collection at the femoral head that extends to the femoral neck. You may also visualize effusions from the lateral position of the patient.
A collection that is not acute may not appear purely anechoic. However, there ought to be asymmetry when compared to the contralateral hip.
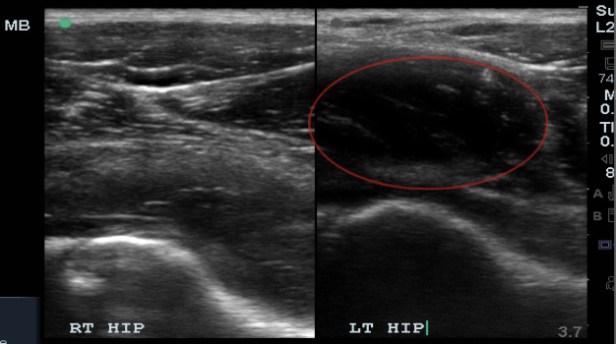
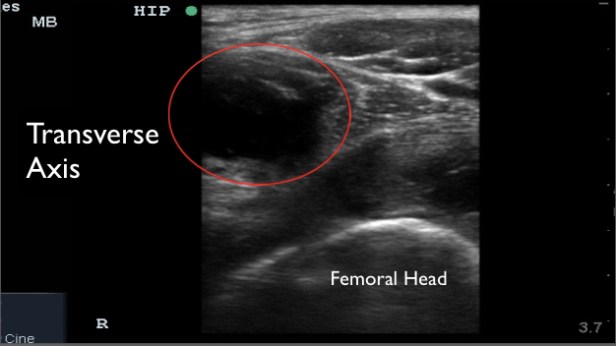
A large mass like collection was identified in this patient. It was initially assumed to be a large joint effusion, but on further evaluation it was less clear if the collection was within the joint capsule or just outside the capsule. I believed the collection was just outside the joint and likely pyomyositis. A radiologist at the bedside believed it was most likely within the hip joint.

Surgery was re-consulted post imaging and they recommended ultrasound guided diagnostic fluid aspiration.
For this procedure, it is important to identify your landmarks and then take note of nearby blood vessels and nerves. I mark the location of the vessels so I am sure to avoid them during the procedure. We used an anterior approach, because the fluid collection was most accessible from this view. Using the high frequency probe, sterile technique, follow a large gauge (18) spinal needle in-plane (longitudinally) and aspirate fluid. In this case, we used procedural sedation.

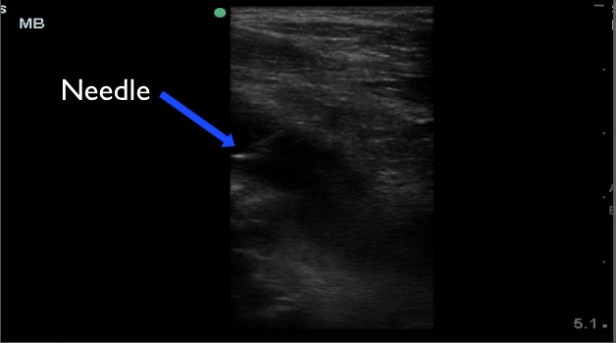
The procedure was completed without issue, but we were unable to aspirate any fluid. The reason is unknown, but likely due to the chronic nature of the infection and the now near solid consistency of the collection.
Without aspiration of fluid the surgeon was not willing to intervene. Another week went by without significant clinical improvement before the surgeon took her to the operating theater. The surgeon identified a large collection of purulent fluid just anterior to the left hip joint, but not within the joint space. It was incised, drained, and irrigated. The patient’s clinical condition improved on antibiotics. Her fevers resolved and she appears well now. Her ambulation improved some and she is using crutches. Unfortunetaly, at the time of this posting her ESR level remained above 100 and a repeat ultrasound showed re-accumulation of the fluid collection. More to come….


Maybe infected iliopsoas bursa. Cool case.
LikeLiked by 1 person